Health inequalities in emerging countries, the case of India
References | citation |  English |
English |  français
français
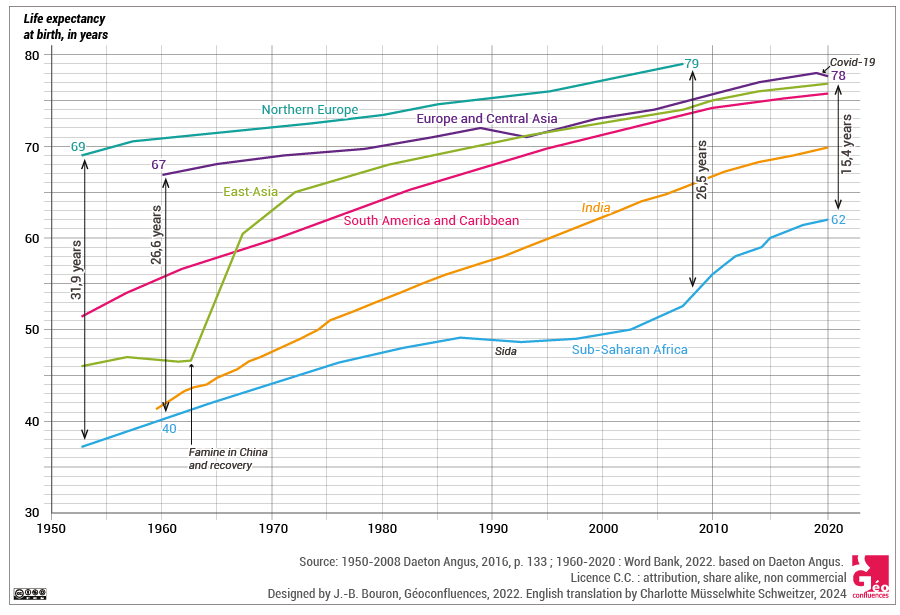
On the global scale, progress regarding reduced death rates and longer life has been considerable since the 1950s. Linked with improved living conditions and medical progress, the average life expectancy grew from 47 years in the 1950s to 73 years in 2019 (71 years for men, 75 years for women) (Pison, 2019). At the same time, although the inequalities between emerging, developing and developed countries remain admittedly very significant, the overall tendency is clearly towards their reduction. Angus Deaton demonstrates that the life expectancy gap between Sub-Saharan Africa and Northern Europe went from 31.9 years in 1950 to 26.6 years in 2010 (Deaton, 2016, cf. Document 1). Since then, life expectancy inequality has kept reducing on the global scale, and the gap separating the region with the lowest life expectancy (Western Africa – 58 years) and the one with the highest (Southern Europe – 82.5 years) was 24.5 years in 2019 (Pison, 2019).
|
Document 1. Life expectancy in different parts of the world since 1950. Source : based on Deaton Angus, La grande évasion. Santé, richesse et origine des inégalités, Presses Universitaires de France, 2016, p. 133. |
Overall, the emerging countries have made the most remarkable progress of all. This dynamic has to be related to their economic growth since the 1980s, which led to a better satisfaction of basic human needs, such as access to food, improved living conditions, developing education and social policies. In Brazil, for instance, life expectancy has thus passed from 66 years in 1991 to almost 77 years in 2019 (Instituto Brasileiro de Geografia e Statística). In the same period, life expectancy in China progressed from 69 to 77 years (World Bank).
|
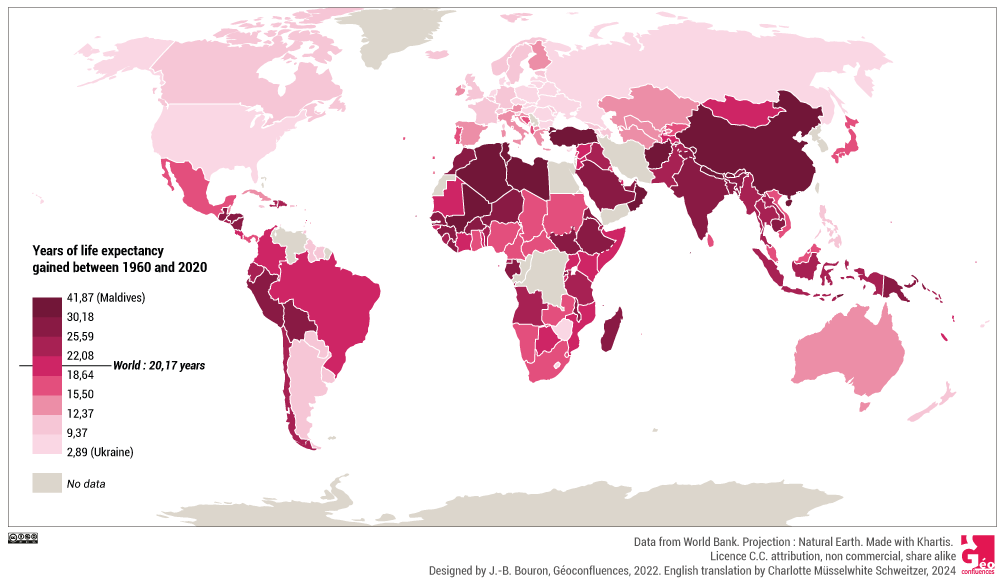
Document 2. Years of life expectancy gained between 1960 and 2020, by country. Data from World Bank, CC BY NC SA. |
Progress is thereby real but needs to be considered with caution and nuance for two main reasons. First, since the 1990s, one will acknowledge, on a global scale, not only the persistence of health inequality, but also the slowing down of its reduction. Furthermore, what is observed on the world scale should not hide local realities which show, on the contrary, not only continuing but even increasing inequality. The aim of this article is to demonstrate that economic growth on its own is not a sufficient condition for optimal health improvement. It will also be a case of re-examining the process leading to the build-up of health inequality, usually addressed from the socio-economic view, with a particular focus on the contributing role of environmental degradation and emerging health issues. In order to achieve this, the scope will draw on the case of emerging countries, the multiple economic and social paths of which provide a good illustration of the complexity in the process of construction of their health inequality. Parmi eux, l’Inde offre une grille de lecture originale qui tient à sa structuration sociale parmi les plus inégalitaires au monde, et aussi aux problèmes majeures de développement auxquels le pays reste confronté malgré la forte production de richesses. Amongst them, India offers an original approach resulting from its social structure which is one of the world’s most unequal, as well as from the major problems of development that the country still has to deal with, despite its great production of wealth.
1. Economic emergence, a necessary but insufficient condition for the improvement of health
The dynamics promoting health inequality are part of a more general movement of a "renewal of global inequality" (Deldrève, 2015) over the past decades, owing to the economic emergence of a number of countries, and to the resurgence of old inequalities, embodied by the unprecedented enrichment of the wealthiest segments of a population whilst at the same time, the standard of living of the less privileged rises little or even falls (Piketty, 2004).
1.1. Health, a sensitive gauge of socio-economic dynamics
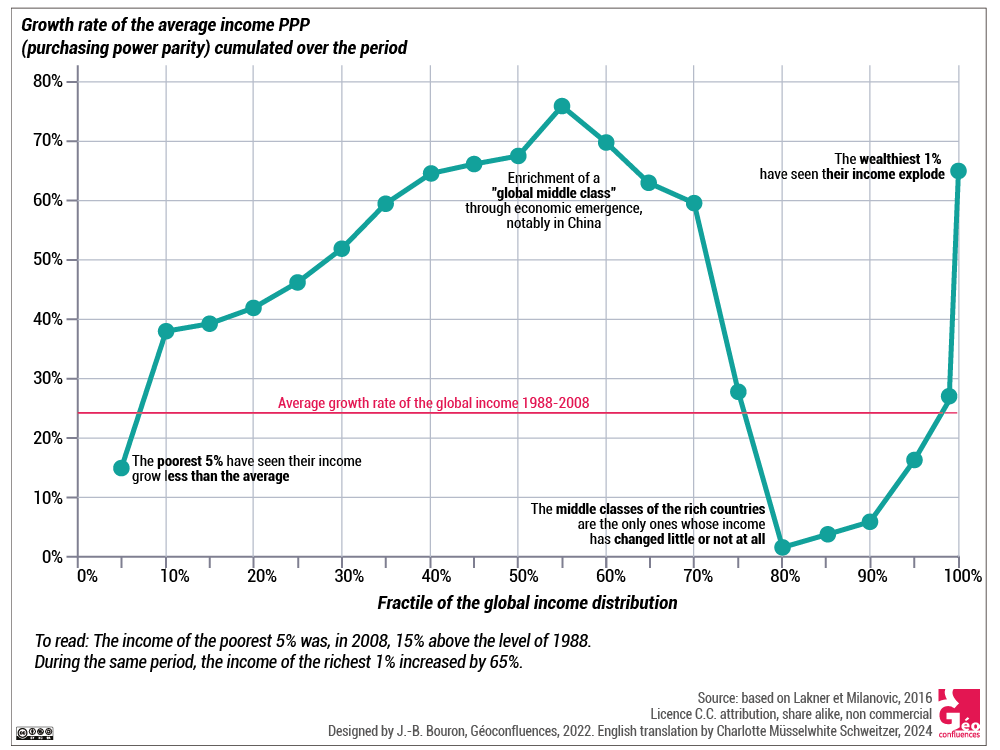
On the global scale, the work of economists Lakner and Milanovic on the profile of income disparities between 1988 and 2008 (Document 3) clearly presents the hubs of economic growth which include the emerging countries, as well as the unequal distribution of produced wealth. The general profile of these income disparities appearing from this economic analysis, known as the "Elephant Curve", highlights first of all the groups that benefitted little from the wealth produced. This applies to both the poorest 5 %, whose revenue has increased but at a slower pace than the global average income, and to the middle classes of the developed countries, whose revenue has stagnated or only marginally increased. In contrast, the middle classes of the emerging countries and the 1 % richest of the planet are the ones who benefitted most from this redistribution of global income (Lakner & Milanovic, 2016; Milanovic, 2019).
|
Document 3. Relative gains in real income, per person and per fractile of the global income (1988 - 2008). This figure, known as "Elephant Curve" due to the shape of the curve reminding of an elephant raising its trunk, brings to light the "winners" and "losers" of global income redistribution in the period from 1988 to the economic crisis of 2008. Based on Lakner and Milanovic (2016), pp. 203-232. |
These economical dynamics shed some light on the evolution of health indicators. In developing countries, the increase of income since the 1950s has contributed to lower mortality, but the situation nevertheless remains critical and the health indicators stay below the global averages (for many reasons, which are related to precarious living conditions). In the developed countries, the economical dynamics at play are one of the factors explaining the persistence of health inequalities that can be observed, due to the significant improvement of health indicators amongst the more privileged on one hand, but the stagnation or even degradation of those factors in the middle and the poorer classes on the other hand. However, it is unquestionably in the emerging countries that health inequalities have deepened the most. This is due to the emergence of a middle class which generally derives substantial benefits from economic growth, whereas the remaining population does not. In the emerging countries the increasing income gap between the different social groups also reveals a complex epidemiological table, characterized by a double burden of ill-health. Indeed, where the health profile of the middle class is coming closer and closer to that of developed countries (regarding life expectancy and causes of death), the health profile of the groups that have been left out of the bounty of economic growth has more traits of underdeveloped societies (lower life expectancy, illnesses due to lack of nutrition, predominant infectious and parasitic diseases).
Describing the unequal distribution of wealth on a global scale helps to understand the evolution of health inequality. It also suggests that although economic growth is essential for improving health, it is nevertheless insufficient if not supported by a fair distribution of produced wealth, as is well illustrated by the case of India.
1.2. Is there a projected roadmap of development favouring health in India?
India makes for an enlightening case of the effects of insufficient development on health, and the expression of "growth without development" used by Jean Drèze and Angus Deaton to characterize it has real significance. Effectively, life expectancy rose sharply after Independence, going from 32 to 58 years between 1951 and 1991 (cf. Documents 1 and 2). However, since 1990, when economic emergence started to accelerate, the rise continued but at a surprisingly slow pace compared to the strong rates of economic growth ((From 1990 to 2015, annual growth fluctuated around 7 and 10 % until it established itself around 5 % per annum until 2019. In 2020, due to the health crisis, India experienced its first recession since it started emerging, with a GDP falling by 7 %. But from the end of the second wave recovery accelerated and GDP should reach 9.4 % in the financial year of 2021-22, before falling back to 8.1 % in 2022-23 and stabilizing itself again around 5 % in 2023-24 (Source: OCDE [OECD] (2021), Perspectives économiques de l'OCDE, vol. 2021, n°2, Éditions OCDE, Paris, https://doi.org/10.1787/09bf9e01-fr).)). So, about 30 years after this economic growth started, life expectancy increased less than before and remained at a level below the global average and of other emerging countries. Indeed, according to the latest Indian census, life expectancy was 67.9 years for the period of 2010-2014. More recent estimates from the World Bank point to a life expectancy of around 70 years in 2019. Life expectancy has thus kept increasing, but remains at a lower level than the global average (73 years in 2019).
|
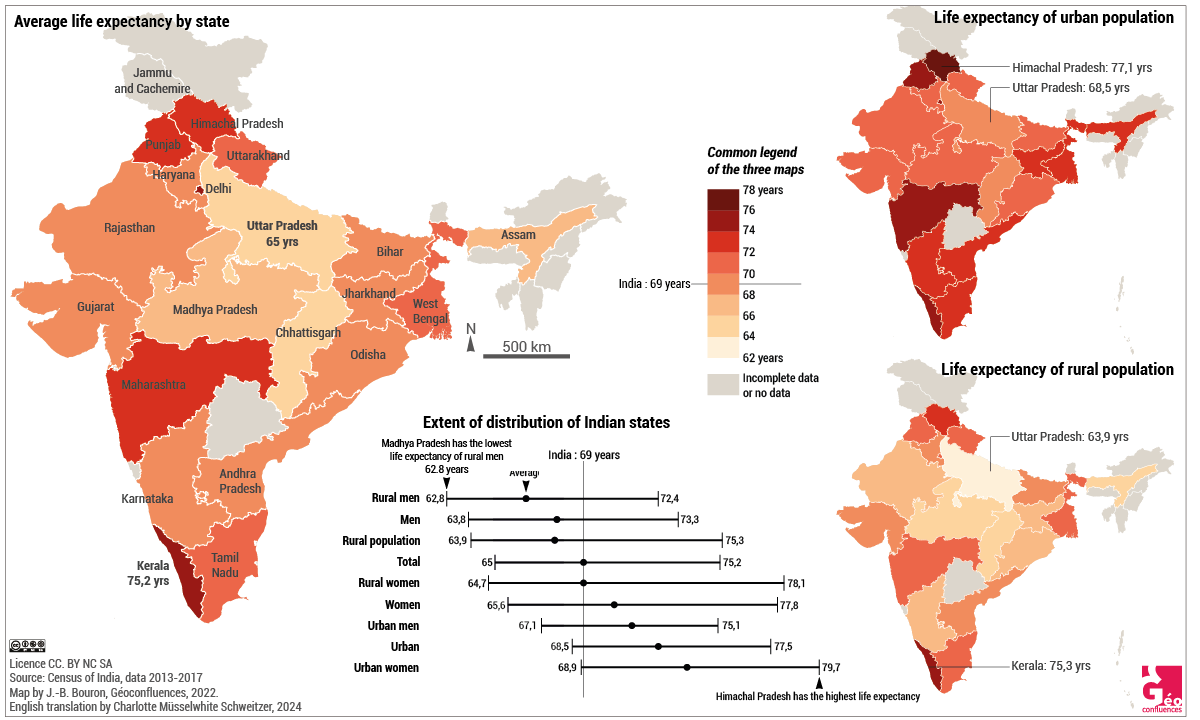
Document 4. Life expectancy in India by state, rural and urban. The data of 2013-2017 are the latest available at the date of realising this chart, waiting for the figures of the 2021 census which was delayed by Covid-19. |
Furthermore, life expectancy in India is still deeply marked by significant inequalities, both regional and social (Document 4). Regarding the former, there was, in 2011, an 11 year gap, between the state with the highest life expectancy, Kerala (74.9 years) and Assam, where it is the lowest (63.9 years). Equally significant is the gap between urban (71.5 years) and rural zones (66.7 years). Same picture regarding infant mortality, which is of 45.4 ‰ in rural zones, against 28.5 ‰ in urban areas (National Family Health Survey IV - 2015-16). Concerning social inequalities, in 2011-2015, life expectancy at birth was 65.1 years for the quintile of the poorest households, against 72.7 years of the wealthiest quintile (Asaria & al., 2019). Along the same lines, a woman of the upper caste lives on average 15 years longer than a dalit woman (Basu, 2020), and child mortality remains higher in lower castes (45.2 ‰) and tribal populations (44.4 ‰), whereas the national average lies at 40.7 ‰). Another remarkable observation is the small gap in life expectancy between men and women, which is respectively 67.8 and 70.4 years in 2013-2017. Indeed, in a classic mortality model, this gap would usually be in favour of women and should be well above 2 years. This is due to the extreme gender inequality still existing in India, which translates to a lifelong female vulnerability in health matters (less attention during childhood, less access to care, insufficient pregnancy follow-up, heavy workload ...).
Thus the improvement of health indicators since Independence is still impacted today by persisting difficult living conditions for a large part of the population and by enduring inequalities. This shows clearly that if economic growth is not accompanied by a fair redistribution of produced wealth, the social benefits, especially in terms of health improvement, lag behind what could rightly be expected. The reduction of social inequalities proves to be of crucial importance to health. This issue is all the more acute, because, where economic growth would naturally favour health (rising living conditions, development of health infrastructure, medical progress ...), it can also jeopardise it because of its environmental consequences. This is a fundamental aspect, as environmental degradation has a double impact on health. There is first the direct effect of health risks to which populations are exposed through environmental degradation (pollution, nuisances, climate changes). There is also an indirect effect, as environmental degradation deepens social inequalities. In order to correctly assess health inequalities, it is important to not just analyse the determining factors in a classic socio-economic way, but to also put other issues into perspective, one of which is that of environment.
2. Health inequalities exacerbated by environmental degradations
In India, and elsewhere, economic growth comes with strong pressures on the environment, in urban as well as in rural areas. Although no one can escape environmental deterioration, its impact on health is socially differentiated, some parts of the population being more exposed and more sensitive to it. Consequences are also social, as environmental degradation contributes to lasting poverty and to reproduction of social inequality ((In India, whatever indicators being used, they all certify a maintained mass poverty. In 2005, the World Bank evaluated at 41.6% the part of population living below the poverty line (1.25 dollars for daily income). In 2010, The Oxford Poverty and Human Development Initiative has suggested a multidimensional poverty index and quoted at 55% the part of the Indian population living below it. In 2019, the United Nations estimated that 364 million people lived in poverty (i.e. 29% of the population).)).
2.1. Environmental consequences of economic growth and differentiated vulnerability of health
In India, sources of environmental degradation are manifold, some are related to the economic trends of the country and to its production models (intensive agriculture consuming much water and phytosanitary products, strong dependency on coal to produce energy ...), others to the insertion into the global economy and the pursuit of higher productivity (heavy drain on natural resources, insufficient and poorly enforced environmental regulations ...).
The rising living conditions of a section of the population also contributes to environmental deterioration through higher consumption (food, car, information and communication technologies...) and the subsequent growing ecological impact. For example, despite still low vehicle ownership in India at 19 cars per 1000 inhabitants (against 140 cars in China and 800 in the USA), a catching-up dynamic can be observed by the increasing car sales ((Le dessous des cartes, « Voiture : l’essor des marchés chinois et indiens », 1er décembre 2019.)). In the same way, the number of smartphone users has risen strongly over the last years, from 34 million in 2010 to 634 million in 2019, and it might reach 920 million in 2025 (GSMA ((GSMA (Global System for Mobile Communications) is an international industry organisation that represents the interests of mobile network operators and constructors worldwide.))).
 |
 |
|
Document 5. Car traffic and plastic pollution in Kolkata. Left: very dense traffic in Kolkata in 2015. Right: plastic on the river Hooghly in 2015. Photograph taken by Virginie Chasles, CC BY NC SA. |
|
Another consequence of increasing consumption is the production of plastic waste. Every year, according to a government source, some 6 million tons of plastic waste are produced. Their recycling being little developed results in an estimated 600 000 tons of unwanted plastic ending up in the Indian Ocean every year, despite the progressive implementation of measures for their reduction (ban of plastic bags and wrappings in the city of Delhi since 2009; ban of single-use plastic items in several parts of the country since 2017). These environmental degradations have already generated proven health issues. The most documented ones relate to air pollution. In this regard, India has some of the most polluted cities of the planet and records the largest number of deaths due to respiratory diseases. In 2017, air pollution was said to have caused 1.2 million cases of premature death in the country. According to the medical journal The Lancet, in 2020 almost 17500 people died in Delhi because of air pollution. In total, the percentage of life lost due to environmental factors in India would be around 19 % (against 5 % in the industrialised countries) (Landy, 2015). It is the poorest category of population that suffers most due to a lifetime of accumulated vulnerability (low income, insecure life conditions, occupational exposure, little access to care ...). For example, their rate of premature death caused by exposure to fine particles (PM 2.5) is 9 times higher compared to the wealthiest categories (Rao, 2021).
Health degradation incidentally maintains the vicious circle of poverty and inequality during the whole lifetime (Aizer & al., 2015). It refers to the term of "poverty trap" and also, more specifically, to the "environmental poverty trap" which stresses the reinforcement of socio-economic and health vulnerabilities generated by environmental deterioration and inequality (Chancel, 2017; Larrère, 2017). This injustice is very real, because the poorest not only fail to benefit from health improving conditions but, what is more, they are much more exposed to environmental degradation, as can be illustrated by the locational rationale of certain polluting activities.
2.2. Do health inequalities reveal environmental injustice?
India's opening to global economy led to developing particularly polluting activities on its land. Amongst those, some are generated byforeign economical players who take advantage of the different levels of development between individuals and territories to maximise their profits. This is then called environmental injustice as certain populations are more exposed to polluting activities than others as a result of less social recognition and the asymetry of power relations.
On the global scale, this can be seen quite clearly through the waste transfer operated from the "North" to the "South". Philippe Billet characterizes this transfer of polluting activities and waste towards developing countries as ecological dumping. As an example, about 50 000 tons of waste electric and electronic equipment (WEEE) arrive yearly in India, mostly from the USA, the UAE and the EU (source : UNO). Some authors hint to a most unequal "waste geography" which produces high risks for the exposed populations (Billet, 2016). This is confirmed by the health data available from the regions receiving large quantities of WEEE. This waste material is mostly unusable, and their primary components, of which some very toxic metals (lead, mercury, cadmium...) are recuperated to be sold. Unsafe working conditions, linked to the absence of strict social and environmental regulations, give rise to major health risks for the workers in these sectors as well as to the neighbouring populations because of the environmental deterioration brought about.
In a similar context one finds the activity of dismantling ships and oil rigs. According to the NGO Robin des Bois, every year a hundred ships arrive in India to be dismantled [5]. The dismantling yards concentrate in the Bay of Alang in the state of Gujarat. This type of activity develops thanks to flexible jurisdiction and bypassing of international jurisprudence. On this subject, ship-owners often resort to flags of convenience to bypass the European law that forces them to decontaminate their ships before they are sent to dismantling [6]. Health and ecological issues are major, as the environment is contaminated by multiple pollutants (lead, mercury, copper, asbestos...), but this sector nevertheless keeps growing for its financial windfall (Tewari & al., 2001).
The importance of health risks related to environmental degradation but also of their aggravation by unequal development cannot be overstated. The same evidence comes from climate change that now affects everybody, but has a stronger impact on the most vulnerable populations' health. In addition to that, the recent experience of the Covid-19 pandemic has also revealed deep inequality in the face of emerging diseases, in respect of death rates and socio-economic effects.
3. Inequalities regarding emerging diseases, the case of the Covid-19 pandemic
The links between health and environment are not confined to health risks due to pollution or climate change. Other challenges are posed as well, emerging diseases for instance, like zoonoses. Their conditions of appearance, propagation and care response are strongly influenced by the levels of development. This was revealed by the Covid-19 pandemic which shed light on inequality in the way it was taken care of, with the possibility of applying social distancing, giving access to vaccination or other indirect effects on health. This inequality, although experienced in a large part of the world, have been found particularly decisive in emerging and developing countries, as will be shown in the case of India.
3.1. Poverty as a major agent for spreading diseases
In India, the effects of Covid-19 are not only explained by the viral virulence and its contagiousness, but also by problems related to development and mass poverty which still define the country. This aspect was visible at different moments of the epidemic, and particularly at its beginning when social distancing was advised to fight the propagation of the disease. Indeed, very rapidly the respect of health measures was compromised by the poor living conditions of a large part of the population. Guilmoto and Licart (2020) have rightly reminded us that basic protective measures like washing hands regularly are impossible for the 40 % of the people who have no access to water and soap, a percentage rising to near 50 % for the lower castes, to 62 % for tribal populations and to 80 % for the poorest households. Another measure that was difficult to apply was social distancing in the face of densely populated homes: according to the 2011 census, about 35 % of urban population live in a single room, proportion that rises to 100 % in the slums.
|
Document 6. Slum neighbourhood in Kolkata along the railway line. Photograph taken by Virginie Chasles, 2015, CC BY NC SA. |
In the same fashion, the cost of facemasks and hydroalcoholic gel is too high for a large part of the population (de Bercegol et al., 2020). The health crisis also highlighted the disastrous effects of the state's slow withdrawal from the health sector and the deficiencies of public hospitals (lack of staff, shortage of beds, insufficient stores of medication and oxygen...). The situation was most critical during the second wave, between March and May 2021. With 400 000 new cases registered daily (four times more than during the first wave), hospitals were overwhelmed. As a large part of the population could not afford to turn to the private sector, many patients died because public hospitals could not take them in. The joint effects of large scale poverty and lacking structures impacted strongly the propagation of the epidemic and its death rate.
3.2. Socio-economic impact of the health crisis and its effect on the death rate
In order to correctly assess the impact of the Covid-19 epidemic in India, one has to take a look at indirect deaths, in particular those related to implemented health measures and to the economic recession caused by the crisis. Regarding the first aspect, it was without doubt the lock-down during the first wave that had the worst effects, as this lockdown had been announced no earlier than four hours before its entering into force on 24 March 2020 (de Bercegol et al., 2020). The economic consequences were a disaster to many employees, among them those of the informal sector (ie 92 % of the working population including agriculture) who were suddenly left with neither income nor allowance.
In India, up to April 2020, fewer people died from the coronavirus than from the effects of lock-down (migrants dying from fatigue or dehydration, adults and children dying from hunger, suicides by fathers of debt-ridden families, victims of road accidents among the migrants...) (Landy et Noûs, 2020). These indirects deaths are still ongoing today, hinting at a deep degradation of living conditions within a large population. Social inequality in direct mortality linked to Covid-19 is being more and more documented, such as a study carried out in the city of Chennai which revealed a higher death rate within the poorest communities (Lewnard et al., 2021).
Conclusion
The health challenges that India has been facing demonstrate clearly that economic emergence alone is not sufficient to create better health conditions for the population if it is not combined with the improvement of living standards. It also shows that social inequality acts as an amplifier. This is a major issue, the more so in a context of environmental degradation that increases the populations' vulnerability and deepens inequality. Indeed, far from equalising human beings in the face of a common danger, environmental changes contribute, to increasing social inequality in general, and health inequality in particular. Addressing these sheds a light on social and environmental issues that societies are facing.
References
- Aizer, A., Curie, J., Simon, P., Vivier, P., 2015, Lead exposure and racial disparities in test scores, Brown University Working Papers.
- Asaria, M., Mazumdar, S., Chowdhury, S., Mazumdar, P., Mukhopadhyay, A., Gupta, I., 2019, « Socioeconomic inequality in life expectancy in India », BMJ Global Health, 4:e001445.
- Basu, T., 2020, Time to Care: Wealth Inequality and Unpaid Care Work for Women in India, Oxfam India.
- Billet, P., 2016, « La régulation imparfaite des injustices environnementales : l’exemple des transferts internationaux de déchets », in Harpet, C., Billet, P., Pierron, J.-P. (dir.), Justice et injustices environnementales, L’Harmattan.
- Chancel, L., 2017, Insoutenables inégalités. Pour une justice sociale et environnementale, Editions Les Petits Matins/ Institut Veblen.
- De Bercegol, R., Goreau-Ponceaud, A., Gowda, S., Raj, R., 2020, « Confiner les marges, marginaliser les confins : la souffrance des oubliés du lockdown dans les villes indiennes », EchoGéo [En ligne], Sur le Vif, mis en ligne le 14 mai 2020.
- Deaton, A., 2016, La grande évasion. Santé, richesse et origine des inégalités, Presses Universitaires de France.
- Deldrève, V., 2015, Pour une sociologie des inégalités environnementales, Editions Scientifiques Internationales Peter Lang.
- Guilmoto, C., Licart, T., 2020, « India and coronavirus : lack of access to handwashing facilities among poor makes fight even harder », The Conversation France, 01 avril 2020.Lakner, C., Milanovic, B., 2016, « Global Income Distribution: From the Fall of the Berlin Wall to the Great Recession », The World Bank Economic Review, 30 (2).
- Landy, F., 2015, Dictionnaire de l’Inde contemporaine, Armand Colin.
- Landy, F., Noûs, C., 2020, Frédéric LANDY, Camille NOÛS, 2020, « Ce que nous dit la COVID-19 des injustices spatiales en Inde », Justice spatiale/Spatial Justice, 15 septembre.
- Larrère, C., 2017, Les inégalités environnementales, PUF, collection La vie des idées.
- Lewnard, J. A., Mahmud, A., Narayan, T., Wahl, B., Selvavinayagam, T. S., Mohan C. B., Laxminarayan, R., 2021, « All-cause mortality during the COVID-19 pandemic in Chennai, India: An observational study », The Lancet Infectious Diseases, S1473-3099(21)00746-5.
- Milanovic, B., 2019, Inégalités mondiales. Le destin des classes moyennes, les ultra-riches et l’égalité des chances, Editions La Découverte.
- Piketty, T., 2004, L’économie des inégalités, La Découverte.
- Pison, G., 2019, « Tous les pays du monde », Population & Sociétés, n°569.
- Rao, N. R., Kiesewetter, G., Min, J., Pachauri, S., Wagner, F., 2021, « Household contributions to and impacts from air pollution in India », Nature Sustainability, n°4.
- Tewari, A., Joshi, H., Trivedi, R., Sravankumar, V., Raghunathan, C., Khambhaty, Y., Kotiwar, O., Mandal, S., 2001, « The Effect of Ship Scrapping Industry and its Associated Wastes on the Biomass Production and Biodiversity of Biota in in situ Condition at Alang », Marine Pollution Bulletin, 42(6).
Virginie CHASLES
Full professor in geography, université Jean-Monnet de Saint-Étienne, UMR 5600 EVS — environnement, ville, société
Translated from French by Charlotte MUSSELWHITE-SCHWEITZER
Web layout : Jean-Benoît Bouron
Pour citer cet article :Vaimiti Goin, « L’espace indopacifique, un concept géopolitique à géométrie variable face aux rivalités de puissance », Géoconfluences, octobre 2021. |
Cite this text:
Virginie Chasles, « Health inequalities in emerging countries, the case of India », Géoconfluences, October 2021. Translated from French by Charlotte Musselwhite-Schweitzer in April 2024.
URL: https://geoconfluences.ens-lyon.fr/programmes/dnl/dnl-hg-anglais/health-inequalities-emerging-india
Pour citer cet article :
Virginie Chasles, « Health inequalities in emerging countries, the case of India », Géoconfluences, avril 2024.
http://geoconfluences.ens-lyon.fr/programmes/dnl/dnl-hg-anglais/health-inequalities-emerging-india


 Mode zen
Mode zen